Performance Report
Your safety is our priority
Clinical Outcomes
Overview 2024
Cardiothoracic Surgeries
| Coronary Artery Bypass Grafting (CABG) | 1,507 |
| Valve Surgery | 365 |
| Valve + CABG (Combined) | 166 |
| Aortic Surgery (Vascular surgery) | 428 |
| Congenital Heart Surgery Simple & Complex | 800 |
| Thoracic Surgery | 178 |
| Specialty Cases + Others | 1,119 |
General Cardiology Procedures
| Diagnostic Procedures | 12,496 |
| Interventional Procedures | 4,785 |
| Electrophysiology | 1,895 |
| Implant Procedures | 864 |
Surgical Overview
Total Volume of Cardiothoracic Surgeries 2022 (N=4,447), 2023 (N=4,476) & 2024 (N=4,563)
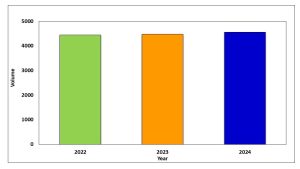
In 2024, IJN surgeons performed a total of 4,563 cardiothoracic surgeries including:
- Coronary Artery Bypass Grafting (CABG)
- Congenital Heart Surgery
- Heart valve repair and replacement
Open And Closed Heart Surgeries
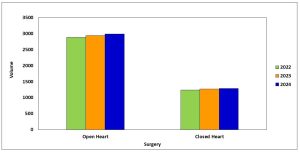
In 2024, IJN surgeons performed 2,986 open heart surgeries and 1,290 closed heart surgeries:
- Open Heart: CABG, Congenital Heart surgery, Heart valve repair and replacement, Aortic root surgery
- Closed Heart: Thoracic surgery, Vascular surgery, Patent Ductus Arteriosus (PDA) ligation, Blalock Taussig (BT) Shunt, Coarctation repair
Cardiothoracic Surgeries by Category for 2024
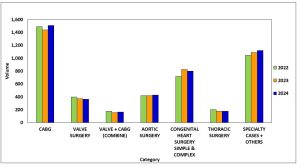
Total Number of Cardiothoracic Surgeries
| No | Categories | 2022 | 2023 | 2024 |
| 1 | CABG | 1,489 | 1,440 | 1,507 |
| 2 | Valve Surgery | 398 | 371 | 365 |
| 3 | Valve + CABG (Combine) | 178 | 156 | 166 |
| 4 | Aortic Surgery | 418 | 418 | 428 |
| 5 | Congenital Heart Surgery Simple & Complex | 716 | 823 | 800 |
| 6 | Thoracic Surgery | 204 | 179 | 178 |
| 7 | Specialty Cases + Others | 1,044 | 1,089 | 1,119 |
| Total | 3,991 | 4,447 | 4,563 | |
Risk Factors for Cardiac Surgeries (N = 6,146), 2022 – 2024
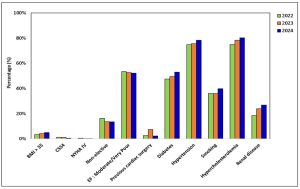
Patients with a complex medical background present greater challenges for cardiac surgery. Almost half the patients had diabetes mellitus at time of surgery, and more than two thirds had hypertension and hypercholesterolemia.
In 2024, patients who have had cardiac surgeries had more complex backgrounds than patients at comparable hospitals as evidenced by higher EuroSCORE – Parsonnet average risk scores.
Actual And Predicted Survival Rates For All Types Of Open Heart Surgeries
All operations
The survival rate for all open-heart surgery was 97.1% in 2024, which is better than the predicted survival rate estimated by the EuroSCORE and Parsonnet scoring system.

Isolated Coronary Artery Bypass Grafting (CABG)
The survival rate for isolated CABG surgery was 97.8% in 2024, which is better than the predicted survival rate estimated by the EuroSCORE and Parsonnet scoring system.

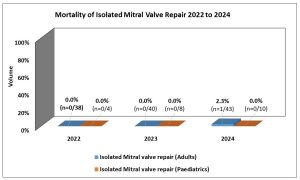
Mortality Rate for Isolated Mitral Valve Repair, 2022 to 2024 (Total no. of Isolated Mitral Valve Repair patient, N=143)
Mitral Valve Repair is preferred over valve replacement whenever suitable. We report that there was no death (mortality) for patients undergoing mitral valve repair from 2022 to 2024.
Mortality Rate for Ventricular Septal Defect (VSD) and related procedures, 2022 - 2024
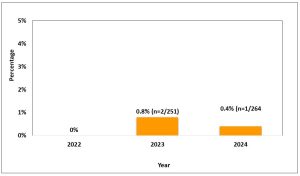
VSD Closure is the commonest surgery for acyanotic congenital heart defects. The death (mortality) rate for simple VSD closure is 0.4% in 2024.
Total Number of Procedure:
| No. |
Procedure |
2022 |
2023 |
2024 |
| 1. | VSD Closure | 249 | 251 | 264 |
*VSD closure – RACHS-1 SCORE 2
Mortality Rate for Tetralogy of Fallot (TOF) Correction and related procedures, 2021 - 2023
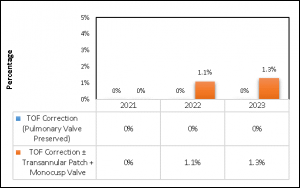
TOF correction is the most common surgery performed for cyanotic congenital heart defects. The death (mortality) rate for simple TOF correction is 1.3% in 2023.
Total Number of Procedure:
| No. |
Procedure |
2021 |
2022 |
2023 |
| 1. | TOF Correction (Pulmonary Valve Preserved) | 39 | 31 | 37 |
| 2. | TOF Correction ± Transannular Patch + Monocusp Valve | 44 | 59 | 42 |
| Total |
83 |
90 |
79 |
|
Ischemic Heart Disease – Interventional Treatment
IJN is the regional and national referral center for percutaneous coronary intervention (PCI). A total of 20,040 cardiac catheterization procedures were performed in 2024 to treat patients with simple and complex ischemic heart disease.
* Source of Data: Cardiac cath procedure from Invasive Cardiovascular Laboratory (ICL)
Use of Appropriate Process Measures: Medications (N = 3,658), 2021 – 2023
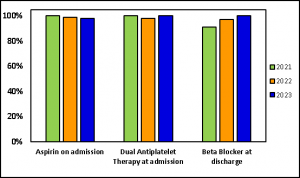
One of the key performance measures is the use of appropriate medications before and after PCI.
From year 2021 to 2023, IJN achieved 98% use for all medication categories, which is comparable with ACC-National Cardiovascular Data Registry (NCDR).
*Source of data: Cardiology Quality Indicators database
PCI Procedure, In-Hospital Mortality (PCI procedure N = 4,024) 2024
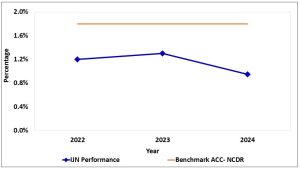
The rate of in-hospital mortality among patients who had PCI procedures at IJN in 2024 is lower compared with ACC- National Cardiovascular Data Registry (NCDR).
Door-to-Balloon Time (N=11,296) 2020 – 2024
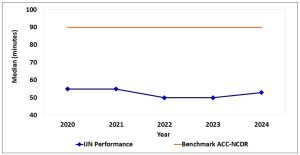
IJN continues to improve door-to-balloon time to reduce the risk of mortality and morbidity, well below the target of 90 minutes for emergency treatment of Acute Myocardial Infarction or heart attacks. (American College of Cardiology/American Heart Association (ACC/AHA) guidelines for PCI inflation).
IJN median door-to-balloon time was 53 minutes in 2024.
Cardiac Catheterization procedures – Use of Radial Access (N= 22,322), 2022 – 2024
In 2024, IJN performed more cardiac catheterization procedures using radial access than other comparable hospitals
(n= 7,612).
The use of radial access is associated with reduction in bleeding complications, readmission rates, infection, and recovery time compared with PCI procedures done using a femoral approach.
Congenital Heart Disease
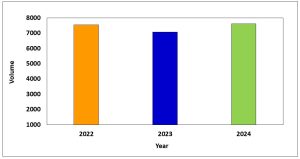
Total Volume of Transcatheter (Non-Surgical) Procedures (N=2,247), 2021-2023
A total of 860 patients had transcatheter (non-surgical) procedures at IJN in 2023.
Total Volume of Interventional Procedures (N=1,050), 2021 to 2023
In 2023, IJN performed 409 interventional procedures for paediatric and adult congenital heart disease patients. The top 6 interventional procedures are; ASD Occlusion, PDA Occlusion, PDA Stenting, Percutaneous Transluminal Balloon Valvuloplasty (PTBV), VSD Occlusion, and Right Ventricular Outflow Tract (RVOT) Stenting.
Note: Numbers show by cases (count by Cath No.), e.g.: Patient undergone for Cardiac Cath and ASD occlusion, case count in “Intervention” group
| No. |
Procedure |
Year |
||
| 2021 |
2022 |
2023 | ||
| 1. | ASD Occlusion | 63 | 60 | 68 |
| 2. | PDA Occlusion | 53 | 36 | 33 |
| 3. | PDA Stenting | 40 | 25 | 53 |
| 4. | Percutaneous Transluminal Balloon Valvuloplasty (PTBV) | 28 | 28 | 37 |
| 5. | VSD Occlusion | 20 | 15 | 21 |
| 6. | Right Ventricular Outflow Tract (RVOT) Stenting | 8 | 6 | 8 |
| Total |
212 |
170 |
220 | |
Paediatric Cardiology Heart Surgery (N=3,529), 2021 – 2023
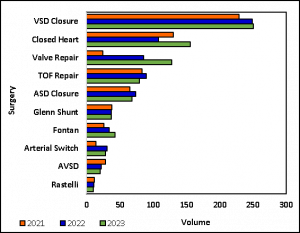
In 2023, IJN surgeons performed 1,105 paediatric cardiac surgeries.
*(Open Heart=949 & Close Heart= 156)
VSD : Ventricular Septal Defect
TOF : Tetralogy of Fallot
ASD : Atrial Septal Defect
AVSD: Atrioventricular Septal Defect
Closed Heart:
- Patent Ductus Arteriosus (PDA) Ligation
- Blalock Taussig (BT) Shunt
- Coarctation of the Aorta (CoA) Repair
- Pulmonary Artery (PA) Banding
- Permanent Pacemaker (PPM) Implantation
Average Length of Stay for Surgical Procedures of ASD, TOF and VSD, 2021 to 2023
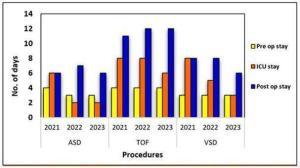
The hospital length of stay for ASD, TOF and VSD were divided into 3 categories:
- Pre-op stay
- ICU stay
- Post-op stay
**ASD: Atrial Septal Defect
TOF: Tetralogy of Fallot
VSD: Ventricular Septal Defect
**Mainly complex and/or very young patients which were not suitable for transcatheter device closure
Length of stay
We at IJN would like our patients to get back on their feet and resume normal life as soon as possible. Therefore, it is our priority to rehabilitate patients and reduce their length of stay.
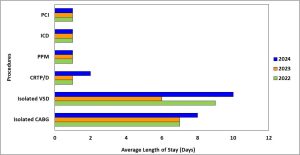
- CABG – Coronary Artery Bypass Grafting
- VSD – Ventricular Septal Defect
- CRTP/D – Cardiac Resynchronization Therapy Pacemaker/ Defibrillator
- PPM – Permanent Pacemaker
- PCI – Percutaneous Coronary Intervention
- ICD – Implantable Cardioverter Defibrillator
Infection Prevention & Control
IJN’s Infection Prevention Program is designed to improve the quality of care through the management of infection prevention, education and research. The Infection Control team collects data on hospital acquired infections and analyses the data to identify patterns and trends.
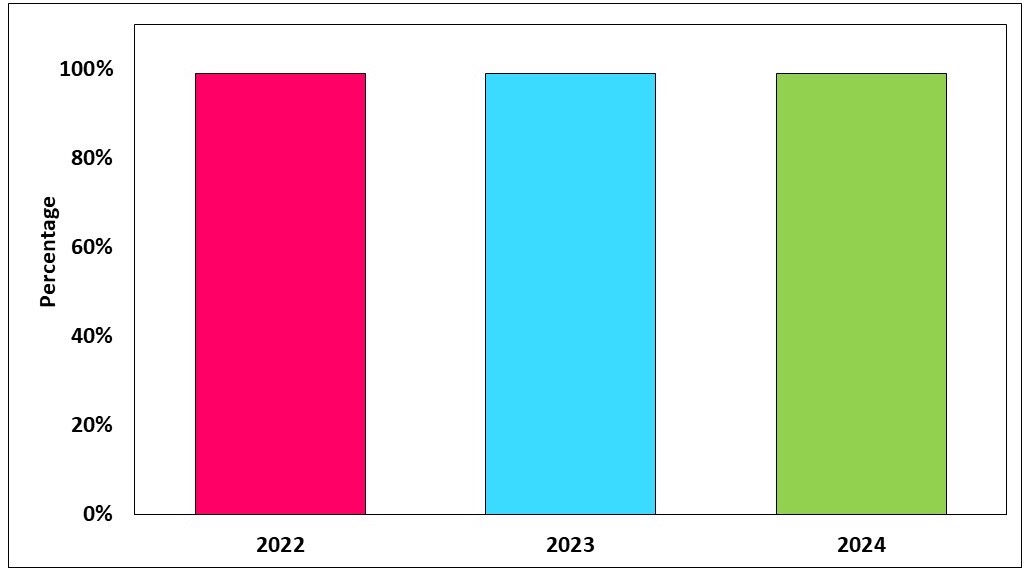
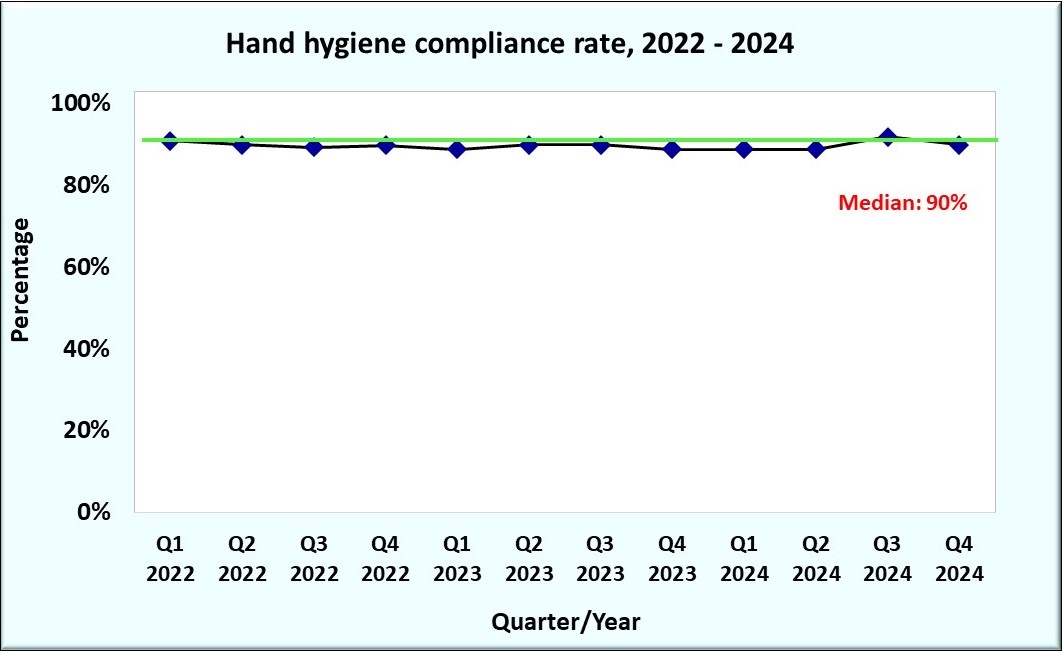
Hand Hygiene Compliance Rate
The graph shows compliance rate by healthcare worker category that includes doctors, nurses and allied health personnel. The annual overall rate has shown a gradual improvement exceeding the Ministry of Health target of ≥75% compliance.
IJN is committed to promoting hand hygiene practice at the point of care amongst our staff.
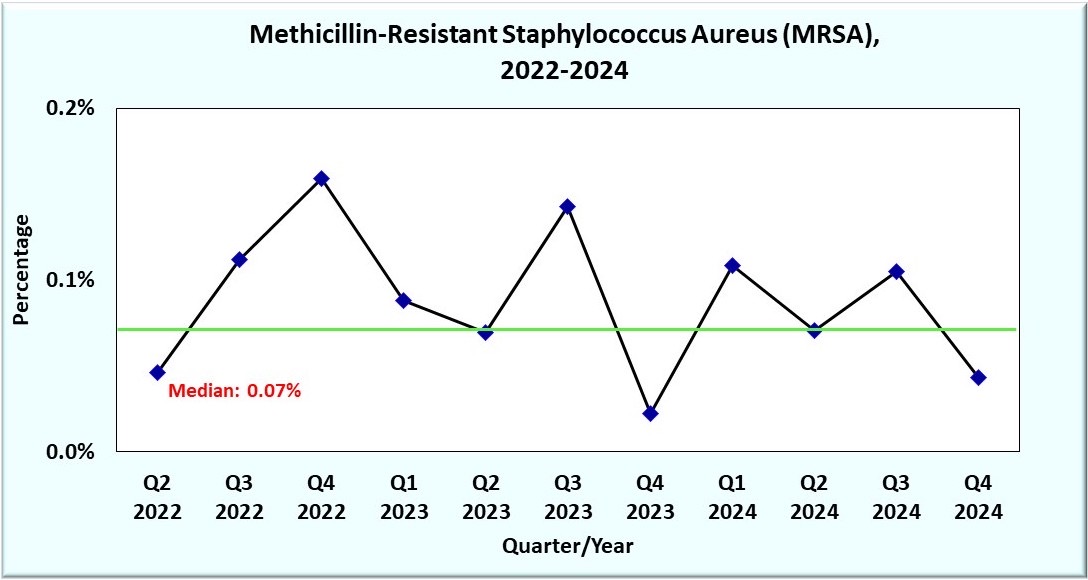
Methicillin Resistant Staphylococcus Aureus (MRSA)
MRSA is a type of bacteria that is resistant to several antibiotics and if left untreated, infections can become severe.
In IJN, the MRSA incidence rate is 0.1% in year 2024.
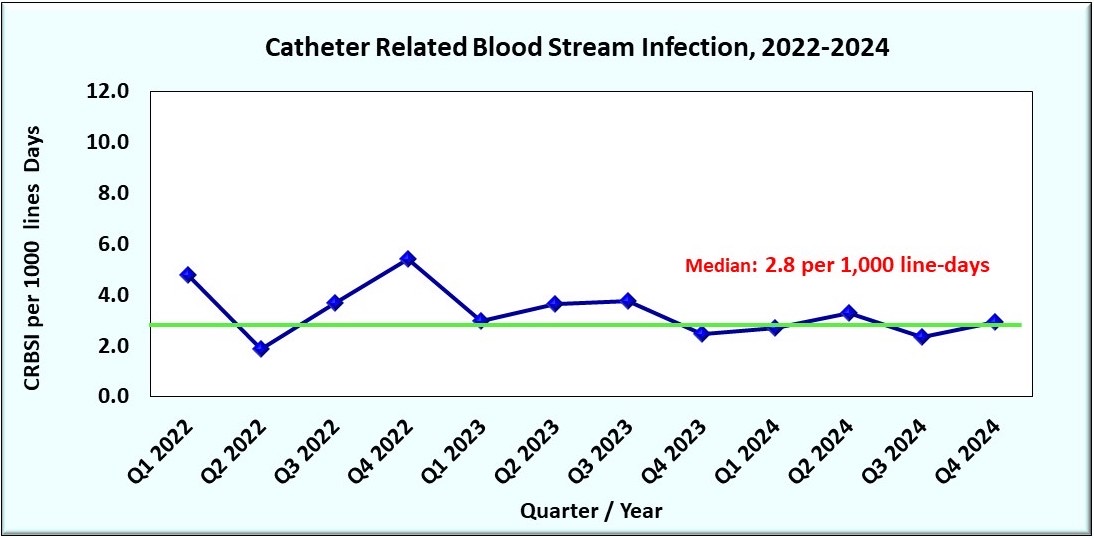
Catheter-related bloodstream infection (CRBSI)
CRBSI is caused by bacteria originating from an intravenous catheter and is the most common cause of a hospital-acquired infection. A dedicated team educates staff and promotes best practices to reduce CRBSI.
We calculate the total number of CRBSI cases against 1000 line-days. In 2024, the CRBSI rate was 2.8 per 1000 line-days.
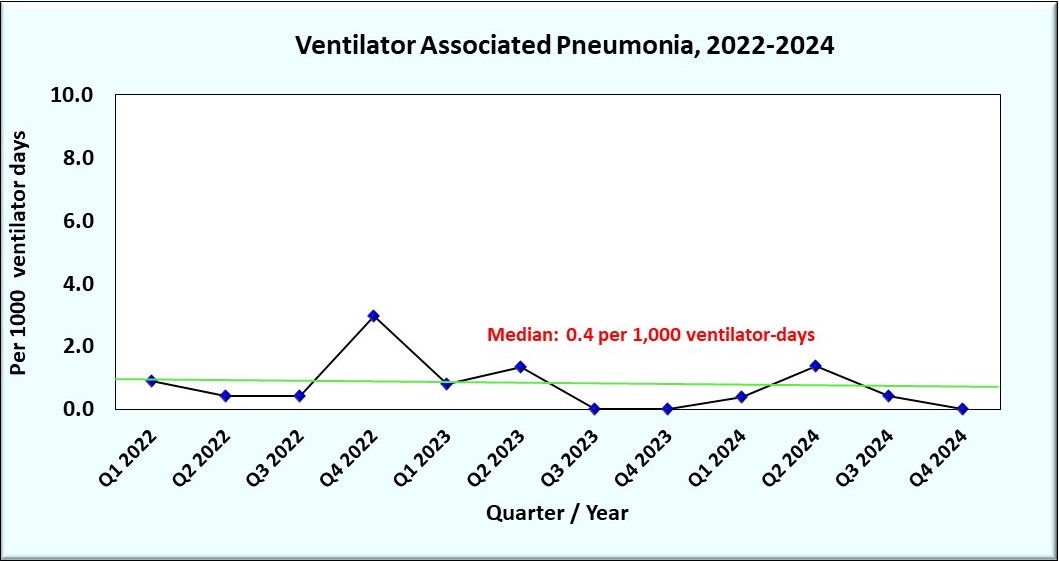
Ventilator Associated Pneumonia (VAP)
VAP is defined as a hospital acquired pneumonia in a patient on mechanical ventilatory support (by endotracheal tube or tracheostomy).
We calculate the VAP rate as total number of VAP cases against 1000 ventilator-days. In IJN, the VAP rate is 0.5 per 1000 ventilator-days in year 2024.
NB: There is no minimum period of time that the ventilator must be in place in order for the pneumonia to be considered ventilator- associated.
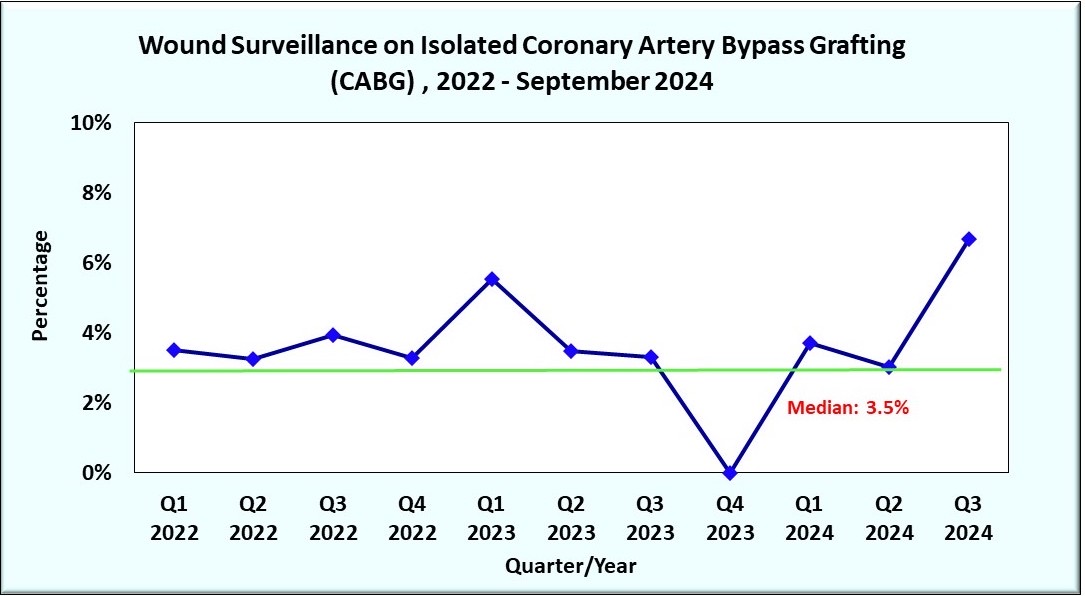
Wound surveillance for Isolated CABG
We monitor the rate of surgical site infection for isolated CABG based on the total number of cases with wound infection against the total number of patients who undergo CABG
From January to September 2024, the average rate of surgical site infection was at 4.5%.
Patient Experience
Your experience at IJN is highly important to us and we continually strive to meet your needs and expectations. Your valuable feedback on our Patient Experience Surveys will help us further improve our services. We identified the results of our Patient Experience Survey based on the response from patients and family members who rated their overall experience in IJN as ‘Excellent’, ‘Very Good’ & ‘Good’.
Inpatient Experience Survey 2022 – 2024
Outpatient Experience Survey 2022 – 2024